In my role as a clinical psychologist specializing in psychotherapy, I am consistently taken aback by the pervasive belief that therapy is a one-size-fits-all solution, applicable to all individuals, regardless of their unique situations. I often come across declarations from fellow mental health professionals asserting that "everyone should be in therapy" and "therapy can benefit anyone." Sadly, this prevailing sentiment often overlooks the very real possibility of therapy leading to unintended negative consequences.
Furthermore, companies like "Better Help" are capitalizing on this misleading portrayal of therapy, offering a watered-down version that falls short of the original intent and potential of therapeutic intervention. This is Capitalism I suppose.
Many individuals embark on their therapeutic journeys without a clear understanding of the substantial variances among therapists in terms of their education, training, expertise, and therapeutic approaches. In the United States, it is not uncommon for people seeking specialized assistance to inadvertently find themselves under the care of a social worker or counselor with limited or no specific training in the precise issues the client is confronting. Shockingly, numerous licensed therapists remain oblivious to extensive bodies of scientific literature that inform evidence-based treatments for specific conditions. This lack of awareness is regrettably quite commonplace.
In certain instances, therapy itself can exacerbate existing conditions or lead to the mischaracterization and mismanagement of presenting problems, inadvertently causing further harm to the client. In this week's article, I delve into some of the typical ways in which therapy can inadvertently result in harm to individuals seeking help.
Providing the Wrong Therapy
Numerous presenting issues pose potentially life-threatening or profoundly disabling challenges. While there remains significant room for advancement in the field, research-backed treatments with essential core interventions do exist. Conditions such as Obsessive Compulsive Disorder, Anorexia and Bulimia, non-suicidal self-injury, and more acute manifestations of post-traumatic stress come to mind.
For instance, consider the treatment of Bulimia Nervosa. A recent study demonstrated that 20 sessions of an active and skill-based Cognitive Behavioral Therapy (CBT) specifically designed for Bulimia (CBT-E) resulted in 42% of participants overcoming binge eating and purging. Remarkably, these patients received just 20 sessions, a stark contrast to the two-year duration of Psychodynamic therapy, where only 15% achieved remission from these harmful behaviors. In reality, the majority of patients are unlikely to receive CBT-E and instead undergo a passive talk therapy, outsourcing the critical work to a medical professional or nutritionist, despite its ineffectiveness. In cases like these, failing to receive the right treatment could be potentially fatal.
Can you imagine grappling with binge eating and purging for several years, yet remaining in the same therapy without experiencing any meaningful progress? Especially when there exists a more effective therapy for your condition? Indeed, those two years of therapy could be considered not just unhelpful, but actually harmful.
Obsessive-Compulsive Disorder (OCD) can be profoundly debilitating, and its most effective approach is a structured behavioral therapy known as Exposure and Response Prevention therapy. OCD is not a condition that typically resolves itself through mere conversation. There's no "eureka" moment that arises from delving into childhood traumas, nor is there a particular dialogue likely to inspire change, and the notion of a "safe space" fostering transformation is often misleading. In fact, such approaches can inadvertently impede the crucial steps required to overcome OCD.
True progress in managing OCD necessitates committed action, skill development, and engagement in a structured therapy regimen with daily homework assignments. Therapy sessions aren't passive discussions but active engagements wherein individuals confront avoided situations and cultivate new coping strategies to better respond to intrusive and obsessive thoughts.In fact, the International Obsessive Compulsive Foundation (IOCF) explicitly identifies ineffective and potentially harmful interventions. To learn more click here
In my years in the field, I have encountered people who have suffered with OCD for years while failing to receive the evidence based treatment for their condition. In fact, they were never even made aware that such a therapy existed. This is harmful!
Effective treatment for conditions like OCD and Bulimia demands specialized therapy delivered by experts who have devoted their careers to the study and treatment of these particular disorders. This same principle applies to the omission of Dialectical Behavior Therapy (DBT) for non-suicidal self-injury or neglect evidence-based treatments for Post-Traumatic Stress Disorder (PTSD).
When therapists extend their practice beyond their areas of expertise, a practice that is unfortunately not uncommon, it can carry the risk of producing detrimental consequences.
Over-Pathologizing Normal Reactions
We find ourselves in an era marked by the medicalization and diagnostic labeling of emotional and behavioral challenges. Contemporary therapists have been trained within a framework that often mirrors the medical profession's approach to categorizing diseases using "symptoms."
In this process, we've inadvertently lost sight of the natural spectrum of responses individuals exhibit in reaction to life's stressors. Instead of enhancing people's capacity to adapt and cope effectively, they are often informed that they possess a "disorder." These labels come with a range of detrimental effects, from individuals self-judging their emotional responses as "aberrant" or "disordered," thereby causing further harm, to the belief that there exists a biological or genetic flaw within them.
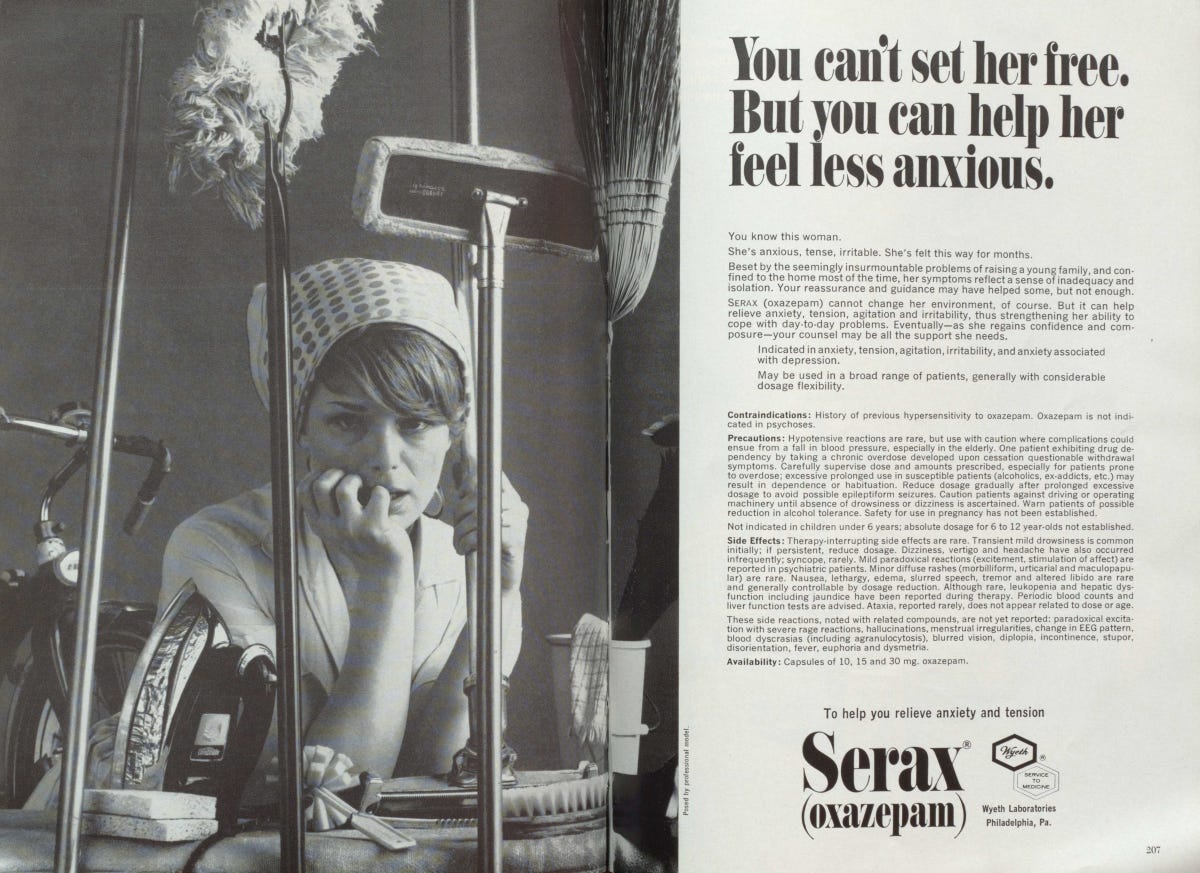
The most alarming consequence of pathologizing these reactions is the tendency to approach them as medical disorders, often resulting in the prescription of one or multiple mood- and mind-altering medications, with the potential for severe and even life-threatening repercussions. Therapists may feel pressured to refer cases to psychiatrists for medical evaluation whenever an individual exhibits a level of distress that falls beyond arbitrary boundaries. This has been reinforced by the misleading notion that combining medication with therapy represents the standard evidence-based approach to mental health treatment.
The outcome of this approach has been unmistakably detrimental, as evidenced by the fact that over 20% of the U.S. population is now taking some form of psychiatric medication, even as mental illness diagnoses and suicides continue to rise. It's crucial to acknowledge that therapy can indeed become harmful when therapists pathologize normal reactions as "mental illness" and guide individuals toward psychiatry.
In my perspective, this issue also appears to stem from a deficiency in receiving a science-based education that establishes a foundation for understanding what constitutes developmentally typical behavior across the lifespan. A significant portion of therapists who provide psychotherapy have completed a Master's level education in fields like social work or counseling. However, this educational background often lacks the essential skills to critically evaluate research, comprehend the intricacies of emotion regulation, or grasp the concept of developmental norms.
Instead, many therapists seem to have succumbed to the trend of commodifying emotional distress by considering it as mere symptoms for the allopathic medical system to medicate. Non-sensical statements such as “it will take the edge off” or it can help you “get more out of therapy” are common place. There is a complete disregard for the harms or how the drug itself can impede progress for what is often a temporary and episodic condition that will resolve itself when the individual faces and overcomes the problem at hand.
It's quite striking that I often observe therapists adopting a perplexingly contradictory stance that leaves their clients confused. On one hand, they ardently champion the value of emotions, validate their presence and wholeheartedly endorsing emotional expression. However, in a jarring twist, they may casually propose psychiatric drugs specifically designed to blunt or numb these very emotions! This glaring incongruity delivers an unmistakable but disconcerting message to clients, implying that their emotions are somehow "too intense" or ill-suited for their current circumstances.
This approach can prove especially detrimental when applied to a spectrum of emotional disorders, encompassing post-traumatic reactions, anxiety disorders, and even grief. The fundamental tenets of these therapeutic methods revolve around the full confrontation and immersion in one's emotional experiences, eschewing any form of evasion or suppression, as this immersion serves as a crucial catalyst for the healing process. We are naturally designed to heal and some therapies actually impede that natural process.
This discordant advice often coerces clients into branding their emotional reactions as "disordered," setting them on a path of self-judgment. Subtly, it steers them away from situations that could evoke those emotions naturally, coercing them into altering their innate coping mechanisms.
These are merely a few of the alarming ways in which therapy can inadvertently wreak havoc, and regrettably, a disheartening number of therapists remain blissfully unaware of these disturbing realities.
Attaching to Clients Stories as Truth
In our field, it is imperative to recognize the inherent danger in unquestioningly affirming an individual's perception of reality, particularly when doing so comes at the expense of rigorous evaluation, critical thinking, and comprehensive case formulation. It is not uncommon for clients seeking therapy to exhibit distortions of reality that significantly impact their clinical functioning.
Currently, there is a prominent debate in the news regarding Rapid Onset Gender Dysphoria in children who present as transgender. This is a relatively recent cultural phenomenon, and the reasons behind this reaction may encompass various factors, including trauma responses, social contagion, normal identity confusion, sexual orientation uncertainty, or genuine gender questioning. Automatically affirming the reality of every individual who enters a therapist's office can potentially be harmful.
Our field is currently witnessing a profound transformation in American culture, and this shift has reverberated into the domain of clinical psychology. What should ideally be a scientific, clinically oriented evaluation, grounded in empirical investigation and informed by our extensive knowledge in developmental and clinical psychology, has devolved into a politically charged battleground. Therapists are now at risk of following ideologically informed guidelines rather than utilize sound science and ethical decision making. The stakes are significant, particularly as gender-questioning teenagers can undergo medical interventions that are permanent and life-altering during a vulnerable stage in their development. The use of puberty blockers, hormones, or surgery carries lasting consequences that a child are not fully equipped to consent to, given their age.
As a clinical psychologist, I've personally observed some unfortunate instances where teenagers and adults have made false accusations of abuse, sexual assault, or discrimination. Some individuals feign psychiatric symptoms for personal gain. Some lie or distort situations for an alternative agenda. This unfortunate reality exists within our field, and therapists who lack critical skills in scientific inquiry, may fail to grasp the full spectrum of psychopathology. Those who have been trained to simply passively affirm and validate an individual's reality without a comprehensive contextual understanding are at risk of inadvertently causing harm.
In today's ever-evolving mental health landscape, many parents find themselves adrift, estranged from their own children as they navigate the enigmatic realm of mental health services. It's alarmingly common for therapists to navigate a murky labyrinth of legal intricacies surrounding confidentiality, often leading to the exclusion of families from the crucial evaluation and treatment process.
Yet, in the realm of ethical and scientifically informed mental health, there exists a deep understanding of the necessity to cross-reference self-reported information. This involves engaging with family members, school professionals, or fellow healthcare experts to form a comprehensive view of the client's struggles. When a therapist falls short of this rigorous evaluation, they unwittingly tether themselves solely to the client's account and their unique perception of reality. In my experience, this occurs quite frequently.
I've come across countless parents seething with frustration because they've never been given the chance to speak with their child's therapist, all while privacy laws are invoked as an insurmountable barrier. Essentially, these parents are coerced into relinquishing their child to a mental health professional and then left with no choice but to cross their fingers and hope for the best, all the while having scant involvement in their child's care. This practice isn't just harmful; it's a bafflingly insane notion that has inexplicably become a cultural norm.
Picture the potential chaos that can ensue when clinical recommendations, treatment, and clinical decisions hinge on unverified claims, distorted truths, or the deliberate withholding of pivotal information within the confines of therapy. In such instances, therapy transcends its healing potential and morphs into a vessel of harm.
Imposing Personal Values and Biases
Therapy constitutes a profoundly personal and intimate relationship between a client and a professional therapist. In this dynamic, the therapist shoulders a weighty responsibility: to adeptly manage their personal biases while upholding the autonomy and self-determination of their clients. This responsibility doesn't require the therapist to adopt a passive, opinionless stance devoid of guidance or intervention, especially when the well-being of the client or others is at stake. On the contrary, the therapist's authenticity plays a pivotal role. Nonetheless, an essential facet of the therapist's role is the recognition of how their own life experiences, biases, and beliefs may potentially interfere with the therapeutic process and, in some instances, cause harm.
Consider, for instance, a scenario where a client seeks therapy to navigate marital problems. If the therapist herself is divorced or currently grappling with relationship issues, there exists a risk that her personal experiences might unduly influence her interactions with the client. This could lead to discussions that overly support the notion of ending the client's marriage, and, in extreme cases, result in the therapist projecting her own issues onto the client. More concerning situations may arise when therapists superimpose their personal values, convictions, or judgments that diverge from the cultural or religious framework of the client and their family.
Confirmation bias, the inclination to selectively seek and employ information that aligns with preexisting views and expectations—essentially cherry-picking information to validate specific points—can severely impair clinical judgment. This bias can infiltrate clinical questioning, causing the therapist to focus disproportionately on areas that validate their deeply ingrained biases.
Take, for instance, the gender bias prevalent in psychiatric diagnoses as a stark illustration of this phenomenon. A considerable number of Borderline Personality Diagnoses are assigned to females, while men are more likely to be labeled with antisocial personality disorder, even when their presentations closely mirror each other. Furthermore, women are disproportionately recommended for psychiatric medication compared to men in similar situations.
In recent times, a new therapy orientation with strong political undertones, known as "social justice therapy," has emerged and made its presence felt in the field. Some therapists have embraced the belief that it is their duty to advocate for a particular ideology deeply rooted in social Marxism and other identity-based political movements.
The convergence of industry demands with the politicization of the field has created an atmosphere where the need for highly specialized training to address ever more specific identities has gained prominence. Regrettably, this trend has the potential to undermine the integrity of the therapeutic process as it increasingly aligns with certain identitarian norms.
For those who may be unfamiliar with this emerging trend, it's crucial to recognize that therapy can evolve into what appears to be a form of political indoctrination, all while masquerading as a pursuit of "justice." In essence, it can involve the therapist imposing their personal values outside the ethical boundaries of the profession in an attempt to effect what they believe to be meaningful social change.
In each of these circumstances, and many others, the potential for harm within therapy looms large.
Misunderstanding and Misrepresenting Ideas
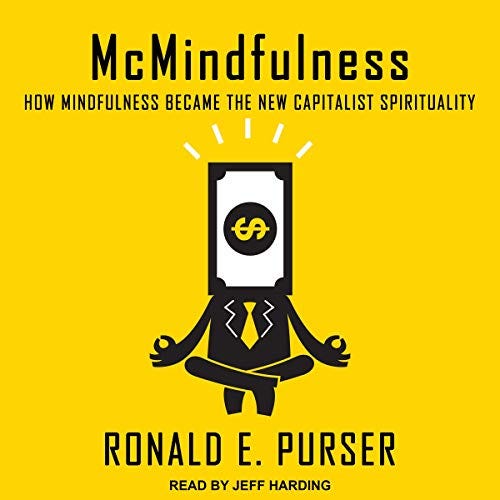
Unfortunately, this is an all-too-common practice, especially among young and inexperienced clinicians. Disturbingly, there's an entire industry that perpetuates the misapplication of scientific findings in ways that can be genuinely harmful. Take, for instance, the trend of mindfulness, which has emerged as an offshoot of ancient Eastern philosophies and meditative practices. While there's no denying that mindfulness is a potent way of life, its powerful potential can be gravely misinterpreted.
Therapists often present mindfulness as a mere "technique" to employ when feeling "stressed," thus twisting its original purpose. This concept gets intertwined with other potentially detrimental mental health ideas. It's crucial to recognize that mindfulness was never intended as an escape or a quick fix for uncomfortable emotions, even though such relief may manifest over time. Rather, its fundamental aim is to heighten awareness and foster a deeper connection with the present moment.
As one can imagine, if the present moment is distressing, practicing mindfulness can intensify that discomfort. This is perfectly acceptable within a therapeutic context that champions the belief that emotions can be fully experienced and harnessed for personal growth. However, when a client is ensnared in a harmful therapy that promotes immediate relief at the expense of learning to regulate emotions and develop effective coping strategies, the entire approach becomes toxic.
It's no wonder many clients exclaim, "Mindfulness doesn't work for me!" as if it were a magic pill designed to instantly alleviate their distress. In reality, it's quite the opposite!
I'll be brief, but the array of issues is extensive. Within the mental health field, there's a notable prevalence of critical misunderstandings and misrepresentations. These encompass misconceptions regarding parent training principles such as reinforcement and punishment, which often result in therapists offering misguided recommendations to parents. Shockingly, many therapists don't fully comprehend the genuine essence of these terms and how they can be employed as effective principles for guiding parent responses. It's disheartening to witness parents unknowingly following therapists' advice that inadvertently reinforces and fortifies the very behaviors they aim to eradicate!
Further, there's the issue of misrepresenting the safety, value, or mechanisms of action of commonly prescribed psychiatric drugs. Pop psychology concepts around "taking care of oneself" sometimes lead to a narcissistic self-focus that hinders the development of healthy relationships. Not to mention the excessive time spent ruminating and discussing specific issues under the guise of "working through something." The world of "therapeutic" settings is rife with psychobabble nonsense that deserves its own in-depth exploration.
Superficial Insight & Manufacturing New Problems
Let's delve deeper into the quagmire of psychobabble that often parades as therapeutic wisdom. One prevailing notion we've concocted is that incessantly discussing one's problems equates to psychological health and therapeutic progress. In certain cases, even for clients who are generally functioning well, they find themselves compelled to scrutinize every facet of their life that might be deemed unfulfilling, all in an effort to generate content for their weekly therapy sessions. This practice is cloaked in the belief that therapy is universally beneficial, akin to a weekly gym session for physical health. But the reality is far from this idealized portrayal.
Forcing oneself to revisit every minor discomfort or challenge can result in superficial insights of limited value. "Not enough 'me time,'" "My partner doesn't fulfill my needs," or "I tend to be a people-pleaser and need to assert myself" are common shallow realizations. These insights often draw from modern Western cultural ideals that posit our happiness is contingent on external factors, whether they be interpersonal relationships or material possessions. Paradoxically, this approach can inadvertently create new problems, perpetuating an endless cycle of topics to fuel the therapy industry.
Creating Dependence
From my standpoint, I firmly believe that therapy should typically have a time limit, aimed at empowering individuals to embrace life more fully by equipping them with new skills and knowledge to enhance their lives. Its core objective should revolve around helping people break free from stagnation, resolve challenging episodes, or conquer debilitating conditions such as OCD, Post-Traumatic Stress, or Eating Disorders. In essence, therapy should serve as a catalyst for clients to gradually become their own therapists, equipping them with the tools and insights needed to navigate life's challenges independently.
Regrettably, the modern therapy industry has inadvertently cultivated a subset of individuals who view therapy as an essential crutch for navigating life's challenges. I've encountered numerous people who subscribe to the belief that therapy should be a lifelong commitment, and they find it difficult to make decisions without seeking approval from their therapists. It's not uncommon to witness individuals who have been in therapy for a decade or even two, with a relationship that has clearly become unhealthy, making it a struggle for them to break free from their therapists' grip.
Therapy takes a harmful turn when these kinds of relationships are facilitated and perpetuated by therapists themselves. Such scenarios often involve aimless therapy, lacking clear objectives and a plan for termination. In these cases, therapy indeed transforms into a source of harm rather than the healing and guidance it was meant to be.
Conclusions
As I write this article, I'm beginning to realize that the subject is so vast and intricate that it could easily become a full-fledged dissertation. Perhaps it's time to dedicate a Radical Genuine Podcast episode to this very topic! There are numerous subtle ways in which therapy can turn detrimental, including the timing of interventions, insufficient session frequency, and other therapist behaviors that can lead to treatment discontinuation or severe ruptures in the therapeutic relationship.
Nevertheless, for the sake of brevity in this article, I hope that the evidence presented thus far encourages people to adopt a more discerning perspective regarding the therapy industry. It's essential to peer beyond the conventional wisdom that's often presented as absolute truth.
Now, with all that being said, I firmly believe that when therapy is responsibly delivered for the specific problems that warrant psychotherapeutic intervention, it has the potential to be profoundly life-changing. The challenge lies in the scarcity of adequately trained treatment specialists, which regrettably forces many individuals into a diluted version of effective therapy provided by clinicians who are not sufficiently prepared to meet their needs.








CBT led me to dissociate. It is a great therapy for the worried well but not effective for anyone with more complex issues whether they be attachment issues, history of abuse or addition, etc. As a millennial whose friends are all in therapy I know few who "graduated." I did ONLY because I found a trained somatic practitioner who knew I could heal, and helped me move from a state of "managing my chronic disorder" to taking responsibility for my life. She did not give me a time limit- again, that's great for perhaps a worried well overachiever! But seeing myself improve for the first time ever was all I needed.