“Repeat a lie often enough and it becomes the truth”
-Joseph Goebbels, Nazi Minister for Public Enlightenment and Propaganda
The illusory truth effect, also dubbed the illusion of truth or reiteration effect, refers to our inclination to accept false information as accurate when exposed to it repeatedly. When evaluating the truth, individuals often gauge information based on its alignment with their existing knowledge or its familiarity. The former is a logical process, as people naturally compare new information with their established truths. Through repetition, statements become more easily processed compared to novel, unrepeated information, leading individuals to perceive the reiterated conclusion as more truthful.
For decades, a uniform message about antidepressant drugs has been consistently delivered to physicians, and by extension, to the public. Specific advertising tactics have been utilized to target the general population.
Antidepressant drugs correct an underlying deficiency in brain chemicals associated with low mood.
Antidepressant drugs are safe and effective because they have been approved by the Federal Drug Administration (FDA). Any adverse reactions are rare and benefits outweigh the risks.
Antidepressant drugs have decades of evidence demonstrating they are superior to placebo in clinical trials.
Antidepressant drugs should be combined with a Cognitive Behavioral Therapy and if therapy is not available the drugs by themselves are just as effective.
Antidepressant drugs can be utilized across a spectrum of psychiatric presentations, including anxiety, obsessive-compulsive disorder, Post-Traumatic Stress Disorder (PTSD), general stress, grief, and eating disorders.
99% of medical professionals and a majority of mental health professionals continue to embrace these five assertions as truths. In actuality, they are blatant falsehoods—deceptive proclamations carefully propagated by pharmaceutical companies to boost their product sales. How did this happen?
History of “Antidepressants”
The history of antidepressants traces back to a serendipitous discovery in the 1950s. Initially developed to find a cure for tuberculosis, chemists experimented with surplus rocket fuel from World War II stockpiles. Two chemicals, iproniazid, and isoniazid, showed promise for destroying bacteria. Although the intended tuberculosis cure failed, researchers observed varying effects on patients' mental states and behavior. The initial drugs had significant adverse effects and high toxicity, necessitating strict regimens and limiting their use. Yet, the concept of influencing mood and behavior by targeting specific brain chemicals with pharmaceuticals emerged.
The Serotonin Hypothesis & SSRI’s
The concept linking clinical depression to deficient serotonin activity in the brain dates back over 50 years, with the initial proposal by British psychiatrist Alec Coppen in 1967. In his review, Coppen considered various factors, including noradrenaline, excess cortisol secretion, and electrolyte disturbances, as potential causes. During Coppen's time, direct investigation of neurochemistry in the living human brain wasn't feasible.
Support for the serotonin hypothesis largely came from the effects of antidepressant drugs, like monoamine oxidase inhibitors and tricyclic antidepressants, which were shown to enhance serotonin action in animal experiments. Coppen cautioned, however, that these drugs' actions might be therapeutic maneuvers unrelated to the root causes of most depression cases.
For centuries, depression was viewed as a malady of the soul, a consequence of hardship. However, a pivotal shift occurred over 50 years ago when scientists, seeking to unravel the biological roots of mood, started conceptualizing depression as a brain disease. This shift coincided with the discovery of biogenic amines, particularly noradrenaline and serotonin (5-hydroxytryptamine, 5-HT), as brain transmitters. This breakthrough paved the way for pharmaceutical companies to create Selective Serotonin Reuptake Inhibitors (SSRI’s) aimed at alleviating the profound suffering of severe depression by increasing the availability of serotonin.
SSRIs mainly target the serotonin transporter (SERT) in the brain, with minimal impact on dopamine transporter (DAT) and norepinephrine transporter (NET). Inhibiting serotonin (5-HT) binding to SERT boosts 5-HT concentration in the synaptic cleft, theoretically improving depression symptoms. Yet, recent systematic reviews have found no correlation between brain 5-HT levels or activity and depressive symptoms. The serotonin hypothesis was never proven.
Drug Manufacturers Design Clinical Trials to Produce Favorable Results
Many consumers are unaware that the U.S. Food and Drug Administration (“FDA”) does not test drugs in the approval process. Instead, drug manufacturers test their drugs and submit their own results to the FDA for review. Hoping to convince the FDA and investors of the safety and effectiveness of their new drug, manufacturers go to great lengths to report positive results in clinical trials.
Several strategies manufacturers use to design clinical trials to make their drugs look better than they are:
Test your drug against a treatment that either does not work or does not work very well.
Test your drug against too low a dose of the comparison drug because this will make your drug appear more effective.
Test your drug against too high a dose of the comparison drug because this will make your drug appear less toxic.
Publish the tests of a single multicenter trial many times because this will suggest that multiple studies reached the same conclusions.
Publish only that part of a trial that favors your drug, and bury the rest of it.
Fund many clinical trials, then publish only those that make your product look good.
While the FDA asks for raw data from clinical trials, it lacks resources to independently verify drug manufacturers' submitted work for accuracy.
Examining the history of SSRIs, it becomes evident that drug manufacturers faced challenges in demonstrating their drug's superiority over placebos. To overcome this hurdle, they utilized the aforementioned strategies to expedite the approval and market presence of their drugs.
Ghost Writing & Hidden Harms
A study published in the Journal of Clinical Epidemiology revealed that a third of meta-analyses of antidepressant studies were written by pharma employees and that these were 22 times less likely than other meta-studies to include negative statements about the drug.
Researchers examined documents from 70 double-blind, placebo-controlled trials of two common types of antidepressants—selective serotonin reuptake inhibitors (SSRI) and serotonin and norepinephrine reuptake inhibitors (SNRI)—and found that the occurrence of suicidal thoughts and aggressive behavior doubled in children and adolescents who used these medications.
They discovered that some of most the useful information was in individual patient listings buried in the appendices. For example, they uncovered suicide attempts that were passed off as “emotional liability” or “worsening depression” in the report itself. This information, however, was only available for 32 out of the 70 trials.
Additionally, another research group reported that after reanalyzing the data from Study 329, a 2001 clinical trial of Paxil funded by GlaxoSmithKline, they uncovered exaggerated efficacy and undisclosed harm to adolescents.
Selling Lies
Drug companies employ extensive advertising, targeting both physicians and consumers, to propagate neuroscientific theories about mental illness. These campaigns aim to persuade doctors and patients that their products possess a clear, objective, and scientific connection to the symptoms they purportedly treat.
In American popular culture, the prevailing perception of mental illness is often simplified—an individual strolling down the street, life seemingly fine, until an abrupt chemical imbalance arises out of the blue. Through direct-to-consumer advertising, drug companies have crafted a straightforward marketing approach, easily comprehensible to the public and readily communicable by physicians. The chemical imbalance lie was born.
This theory significantly fueled the emergence of biological psychiatrists, transforming the psychiatry profession. It shifted the focus from therapies and managing severe mental illness to legitimizing psychiatrists as medical doctors who treat patients' organic diseases. Similar to internists addressing insulin shortages in diabetics, psychiatrists began addressing serotonin deficiencies in depressed patients. Depression was no longer seen as just a natural response to stress, there was now an underlying biological factor which was the cause of the depression.
Pharmaceutical companies found an expanded customer base by normalizing depression and aligning with the psychiatric medical establishment. This allowed them to broaden the diagnosis criteria and market their drugs to a significantly larger audience. They further enlisted academics from prestigious institutions to endorse their drugs at national conferences and produce papers on the drugs' effects, essentially turning them into paid spokespeople. The outcome: billions in annual sales and a considerable expansion of psychiatry's role in American society.
For an expanded look at the corruption I highly recommend this article from Mad in America: Read here
Credit: Mad in America
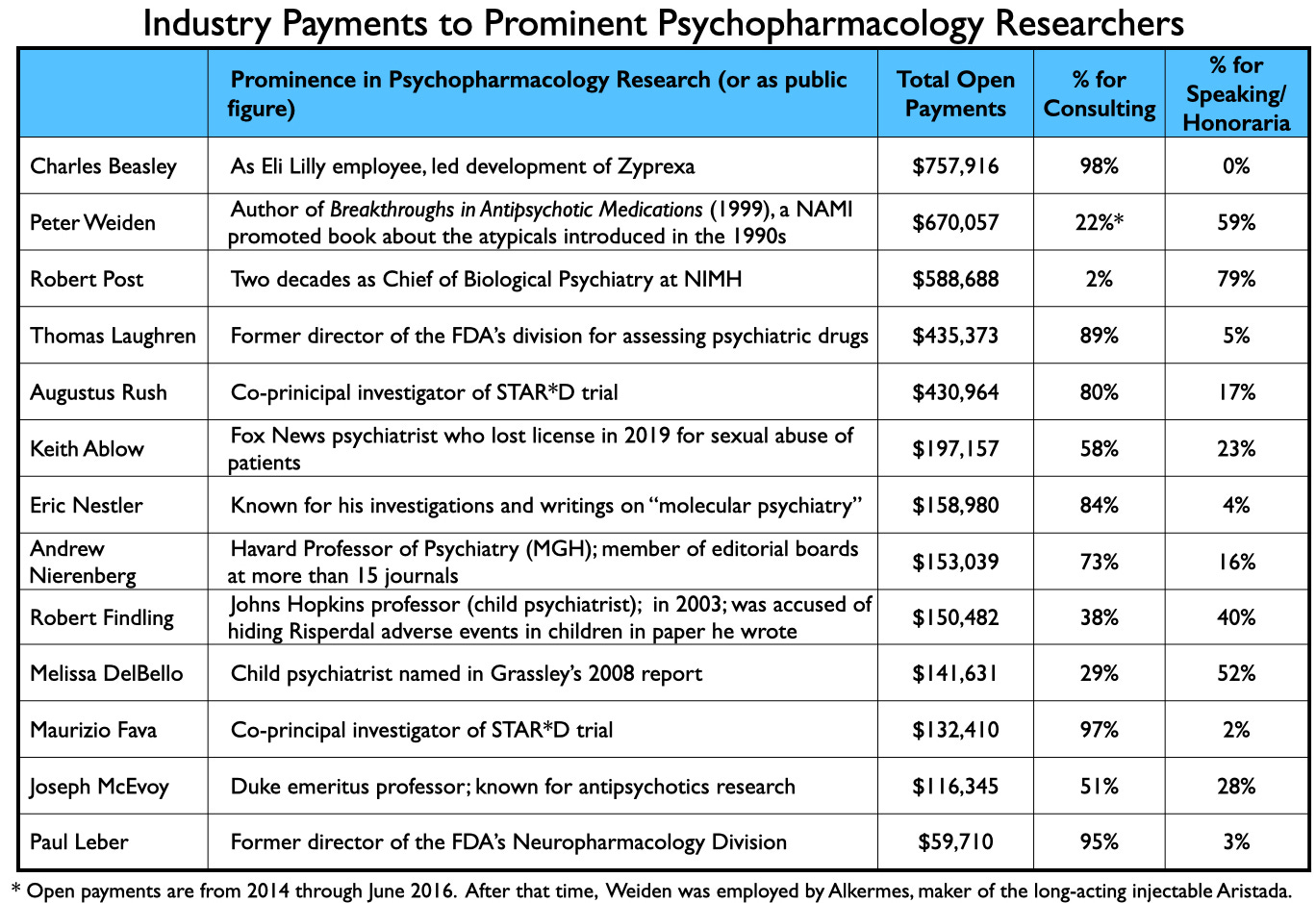
Industry Payments to Prominent Psychopharmacology Researchers: Credit Mad in America
Infiltrate Primary Care & Influence Guidelines
In recent years, there has been growing concern about the infiltration of drug companies into primary care centers, notably to promote psychiatric drugs. Pharmaceutical companies often establish strategic partnerships with healthcare providers, offering educational materials, financial incentives, and even sponsored events to influence prescribing patterns. It is now believed that more than 80% of antidepressant drugs are prescribed in primary care.
Pediatricians, burdened by time constraints, find themselves at a heightened risk of pathologizing normal reactions and succumbing to the pressures of overdiagnosing clinical depression. What's more troubling is that these diagnoses often rely on biased screening measures, conveniently developed by the very pharmaceutical industry that profits from the sale of these drugs.
If you're curious about the potential reasons behind the American Academy of Pediatrics' inclination to amplify the number of children identified as depressed, as well as their willingness to misrepresent scientific literature by overestimating the effectiveness of antidepressant drugs and downplaying their potential risks, it's worth examining their major donors.
The American Foundation for Suicide Prevention receives 63% of its funding from industry. The major donors include: Pfizer, Lilly, Johnson & Johnson, Sanofi, Mallinckrodt pharmaceuticals, Bristol Myers Squibb and other pharmaceutical companies. If you examine the top 10 list of donors (unknown amount of funding) these other companies, foundations and organizations have major ties to the pharmaceutical industry.
Primary care doctors, constrained by time pressures, are increasingly compelled to adhere to industry-established guidelines that advocate antidepressant drugs as frontline, effective, and safe interventions for a range of psychiatric presentations.
How to Reclaim Truth
Advocate for informed consent. It is your legal and ethical right to comprehend the risks and benefits.
Reframe the narrative around psychiatric drugs. Let's call them what they are – drugs, not medicine.
Educate your primary care doctors. They weren't trained to address mental health issues and are unknowingly perpetuating pharmaceutical marketing misinformation. They are operating beyond their boundaries of competence.
Challenge the notion of a chemical imbalance. Depression is not a "brain disease." Dispel these myths to foster a more accurate understanding of mental health.







Excellent. Thank you!
I was diagnosed with ADHD when I was four years old. There's a very good chance I have outgrown the diagnosis. I was prescribed Ritalin back then and I'm on Concerta now. If I had children, based on what I know now, I would be hesitant to put them on medication until I was confident that the diagnosis was true. I have a cousin whose stepdaughter was misdiagnosed with ADHD and Oppositional Defiant Disorder when in reality the problem was is she is a celiac.