Are SSRI's Impacting Gender Identity & Sexual Development?
Exploring the consequences of antidepressant use in adolescence
The widespread prescription of Selective Serotonin Reuptake Inhibitors (SSRIs) to adolescents for depression and anxiety may be unleashing consequences far beyond their intended effects. Despite poor efficacy data and questionable long-term safety profiles in youth, these powerful drugs continue to be dispensed at alarming rates.
We already know of their link to Post-SSRI Sexual Dysfunction (PSSD), a devastating condition that can permanently alter sexual function even after discontinuation. But could the impact of SSRIs be even more profound, potentially reshaping the core of adolescent identity and sexual development?
The surge in SSRI prescriptions for adolescents coincides with an unprecedented rise in gender dysphoria cases, yet the potential link remains largely unexplored. Given our understanding of serotonin's crucial role in sexual development and expression, this correlation demands rigorous scientific investigation.
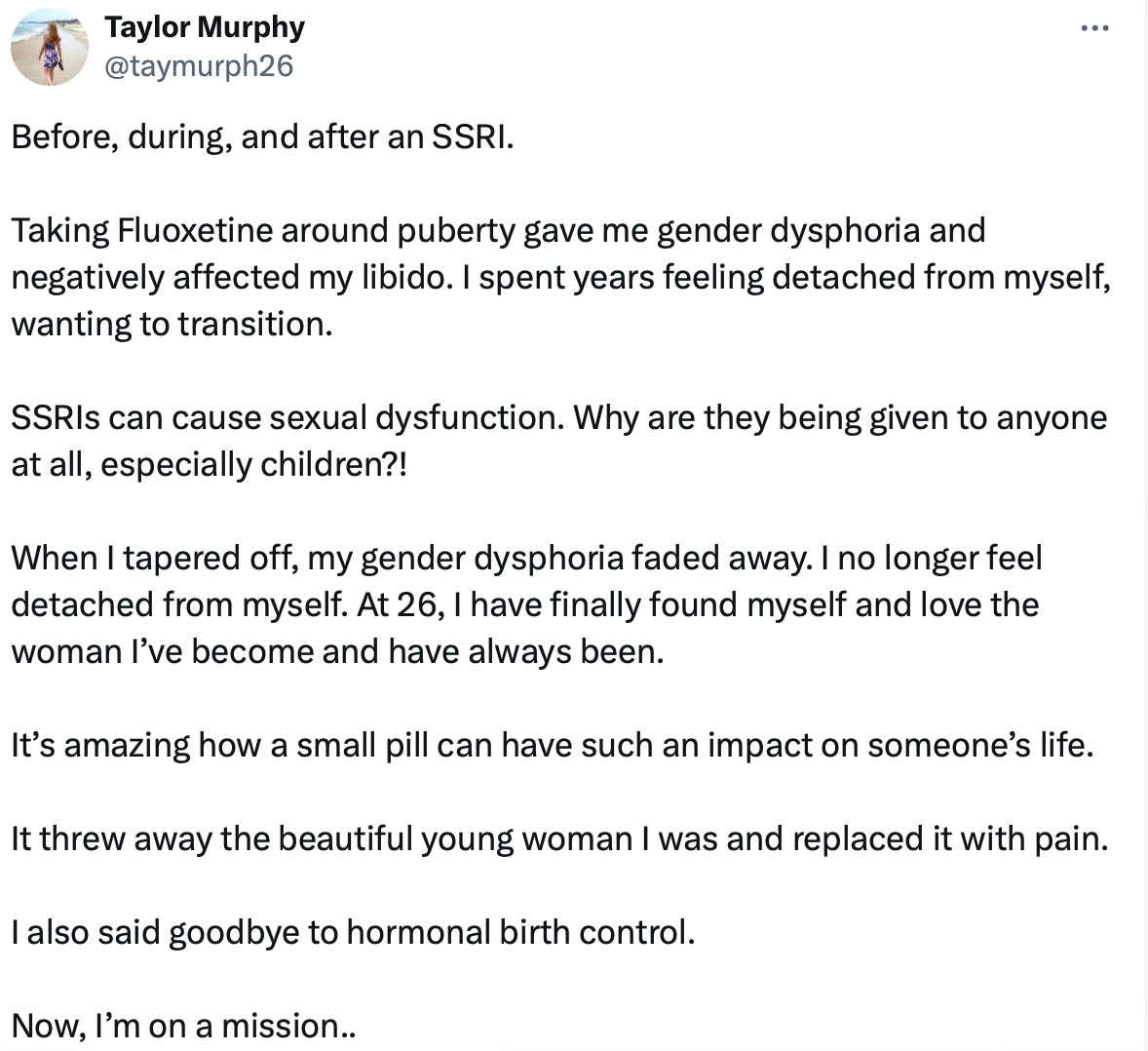
A growing global movement of patients reporting iatrogenic harm from SSRIs is gaining momentum, with many adults now critically examining the impact of these drugs prescribed in their youth. These individuals, prescribed powerful psychoactive medications at a time when they were legally unable to provide consent, are raising alarm bells about the long-term consequences of early SSRI use.
Paralleling this trend, a vocal community of de-transitioners has emerged, challenging the medical and mental health establishments. They argue that during their most vulnerable developmental years, the very systems meant to protect them instead fast-tracked life-altering decisions without adequate safeguards or exploration of underlying issues.
Both groups point to a disturbing pattern: the medicalization of normal adolescent struggles, potentially disrupting crucial developmental processes. Their stories reveal the urgent need for a rigorous reexamination of our approach to youth mental health and gender-related concerns, highlighting the potential long-term risks of pharmaceutical interventions during critical periods of identity formation.
However, this critical area of research faces significant barriers. The politicization of gender issues has created a stifling effect on scientific inquiry, with researchers fearing professional backlash or accusations of transphobia. Moreover, the complexity of gender identity formation and the ethical considerations of studying adolescents further complicate research efforts.
The critical discussion of SSRI efficacy and safety remains largely absent from mainstream discourse. Mainstream media outlets, funded by pharmaceutical advertising, consistently neglect to investigate or report on concerns regarding antidepressant drugs, effectively insulating their key sponsors from public scrutiny.
The pervasive influence of SSRI manufacturers extends beyond media, shaping clinical practice through industry-funded guidelines. Healthcare providers, educated within this framework and having prescribed these drugs for decades under the assumption of evidence-based medicine, struggle to re-evaluate established practices due to entrenched professional and personal beliefs.
Parents, desperate to alleviate their teens' distress, often consent to SSRI treatment without receiving full informed consent or understanding all potential consequences, particularly the profound impact on their child's developing identity and long-term psychological and physical well-being.
The deafening silence surrounding SSRI use in adolescents is more than negligence—it's an ethical catastrophe. We're conducting a vast, uncontrolled experiment during crucial developmental years, the risks of which remain largely unexamined. We must ask the questions that researchers, clinicians, and media have long avoided: What are the true impacts of altering neurotransmitter levels in the adolescent brain? How might these interventions affect identity formation, including sexual and gender expression? Why has there been such reluctance to rigorously investigate these issues?
The SSRI Experiment on Teen Brains
The serotonin hypothesis of depression emerged in the 1960s, gaining prominence in the late 1980s and 1990s. It posits that clinical depression results from a deficiency of serotonin in the brain. This theory conveniently coincided with the development of Selective Serotonin Reuptake Inhibitors (SSRIs).
Despite its widespread acceptance, the hypothesis was based on limited evidence. Early studies showing reduced serotonin metabolites in depressed patients were inconsistent and later challenged. The theory gained traction largely through effective marketing by pharmaceutical companies, rather than robust scientific support.
By the early 2000s, the hypothesis faced mounting scrutiny. Research consistently failed to demonstrate serotonin deficiency in depressed individuals. Yet, despite this lack of evidence, both the general public and many healthcare providers continue to view mood disorders and clinical depression as conditions treatable through pharmaceuticals targeting neurotransmitters like serotonin and norepinephrine.
In 2022, a comprehensive review found no convincing evidence supporting the serotonin hypothesis. Despite this, the theory persists in popular understanding and continues to influence treatment approaches.
The duration of most clinical trials for Selective Serotonin Reuptake Inhibitors (SSRIs) is surprisingly brief. While some long-term observational studies exist, the controlled clinical trials used to establish efficacy and safety typically range from just 6 to 12 weeks.
This relatively short testing period raises questions about our understanding of SSRIs' long-term effects, given that many patients use these drugs for months or years. The discrepancy between trial durations and real-world usage patterns highlights a significant gap in our knowledge of these widely prescribed antidepressants.
The U.S. Food and Drug Administration (FDA) has already recognized the vulnerability of young people to antidepressant side effects. In 2007, the FDA mandated a black box warning on antidepressants, including SSRIs, citing an increased risk of suicidal thoughts and behaviors in individuals under 25. This warning underscores the sensitive nature of brain chemistry during this critical period of development. Despite this acknowledgment of risk in one area, the potential impacts on gender and sexual development have received far less attention
We must critically examine the implications of artificially altering serotonin levels in adolescent brains—an intervention of profound consequence given our limited understanding of this remarkably complex organ.
The human brain, with its intricate network of 86 billion neurons and trillions of synaptic connections, remains largely a mystery. Despite our limited understanding, we've intervened by altering its delicate chemical balance during crucial developmental stages.
Are we inadvertently restructuring developing neural pathways, with possible enduring impacts on personality formation, sexual development, emotional regulation, and cognitive function?
The heightened neuroplasticity during adolescence, typically viewed as advantageous for learning and adaptation, may amplify the risks of our pharmaceutical interventions. This is not merely a transient chemical adjustment; it's potentially a fundamental reshaping of neural architecture.
Serotonin and Sexual Development
The intricate interplay between sex hormones and brain development during adolescence is a delicate balance that shapes cognitive abilities, behaviors, and potentially gender identity. During adolescence, brain development plays a crucial role in shaping traditionally feminine and masculine characteristics.
Serotonin interacts complexly with sex hormones like estrogen and testosterone. These interactions are bidirectional - sex hormones can influence serotonin synthesis, release, and receptor expression, while serotonin can affect the production and action of sex hormones.
Serotonin is the oldest known monoamine neurotransmitter; it has numerous receptors and many subtle functions. For example, activation of serotonin type 1a (5HT1a) receptors enhances sexual desire and lowers the threshold for ejaculation; activation of serotonin type 1b (5HT1b) and 1c (5HT1c) receptors decrease sexual desire and inhibit orgasm; and activation of serotonin type 2 (5HT2) and type 3 (5HT3) receptors impair all stages of sexual response in both men and women. By altering serotonin levels, we may be influencing the delicate balance of sex hormones during this critical period of brain development.
Given serotonin's complex role in sexual function and development, how might SSRI use during adolescence alter biological processes related to gender and sexuality?
Could these neurochemical changes create a biological substrate that interacts with prevailing social narratives about gender, potentially contributing to confusion or uncertainty?
To what extent might SSRI-induced alterations in brain chemistry affect an individual's perception and interpretation of their own gender identity, especially when exposed to diverse gender concepts?
Moreover, the rise of social media and online communities centered around gender identity issues can further complicate matters. An adolescent experiencing SSRI-induced changes in gendered behaviors might encounter online narratives that interpret these changes as signs of a different gender identity, potentially leading to misattribution of their experiences.
In this context, chemical interventions during adolescence may not just be altering brain chemistry, but potentially reshaping the very foundation of gender identity formation. As we continue to prescribe SSRIs to developing adolescents, we must consider whether we're inadvertently contributing to gender confusion in an already complex cultural landscape.
Love, Attachment & SSRI’s
Human emotions fundamentally shape our existence, influencing our perceptions, motivating our actions, and fostering the complex social bonds central to our interpersonal relationships. At the heart of this emotional landscape lies empathy - our ability to understand and share the feelings of others.
This profound capacity serves as the cornerstone of attachment, fostering deep, meaningful relationships and enabling the complex social interactions that have propelled human civilization forward. Empathy allows us to transcend the boundaries of our individual experiences, to feel the joy and pain of others as if they were our own, creating bonds that resonate with the very essence of what it means to be human.
Antidepressants often induce emotional blunting — a lack of feeling for both happiness and sadness. This phenomenon has far-reaching implications. How might this reduced emotional range affect an individual's capacity for social bonding and, consequently, the development of gender and sexual identity?
A pivotal research study revealed alarming findings regarding SSRI use and empathy. Patients prescribed SSRIs exhibited significant decreases in affective empathy—the ability to emotionally resonate with others' experiences. Crucially, neuroimaging showed reduced activity in three key brain regions previously associated with empathy for pain.
This suggests that SSRIs may not only alter mood but also fundamentally change how individuals relate to others' suffering. The implications of such neurological changes, especially in developing adolescent brains, are profound and troubling. If SSRIs are indeed dulling our capacity for emotional connection and pain recognition, we must question their long-term impact on social bonding, relationships, and the very essence of human interaction.
Helen E. Fisher, PhD, a biological anthropologist and researcher maintains that taking serotonin-enhancing antidepressants (SSRIs) impacts the experience of love and attachment. According to Fisher, love is not merely an emotion but "a motivation system, a drive, part of the brain's reward system." Her fMRI studies reveal that romantic love is characterized by high levels of dopamine and norepinephrine, coupled with low serotonin levels. This neurochemical profile, particularly the low serotonin, is responsible for the obsessive thinking often associated with being in love.
By increasing serotonin levels, these medications can blunt emotions, potentially dampening the intense elation and preoccupation characteristic of romantic love. This emotional flattening, Fisher argues, may hinder the development and sustenance of romantic relationships.
Post-SSRI Sexual Dysfunction (PSSD)
A healthy libido is often considered an indicator of good overall health and well-being. Sexual desire is influenced by a complex interplay of physical, hormonal, and psychological factors, and its presence can signal that these systems are functioning well.
Post-SSRI Sexual Dysfunction (PSSD) is a debilitating condition that can occur in individuals who have taken selective serotonin reuptake inhibitors (SSRIs), a common class of antidepressants. This condition is characterized by the persistence of sexual side effects even after discontinuation of the medication. These effects can include decreased libido, erectile dysfunction, genital numbness, inability to orgasm or decreased orgasm intensity, and a general lack of sexual arousal. The number of men and women affected by these forms of sexual dysfunction vary; some studies report that as many as 73% of patients taking serotonin-enhancing antidepressants suffer one or more of these sexual side effects
What makes PSSD particularly concerning is its potential to occur after even short-term use of SSRIs, and its ability to persist indefinitely. Some individuals report experiencing these symptoms for years after stopping the medication, with no sign of improvement. This long-lasting impact can have profound effects on a person's quality of life, relationships, and overall well-being.
The mechanisms underlying PSSD are not fully understood, but theories suggest it may involve long-term changes in brain chemistry, alterations in gene expression, or damage to peripheral nerves. The condition is not widely recognized in the medical community, leading to frequent misdiagnosis and inadequate support for those affected.
Of particular concern is the emergence of PSSD in individuals who were prescribed SSRIs during adolescence. Despite the severity of its impact, PSSD remains under-researched and often overlooked in discussions about the risks associated with SSRI use. This lack of awareness means that many patients are not properly informed about this potential side effect when prescribed these medications, raising significant ethical concerns about informed consent, especially when it comes to prescribing SSRIs to adolescents.
Throughout my career as a clinical psychologist, I've encountered a concerning pattern among young adults in their early to mid-twenties. Many report a profound lack of sexual desire and preference, with some identifying as asexual while others express deep shame over their absent libido, often attributing it to "chronic depression."
This widespread lack of awareness about the potential long-term sexual consequences of SSRI use, particularly the risk of Post-SSRI Sexual Dysfunction (PSSD), likely contributes to severe under-reporting of the condition. Patients experiencing persistent sexual issues may attribute their symptoms to ongoing depression or other factors, never connecting them to past medication use. Healthcare providers, often uninformed about PSSD themselves, may reinforce this misattribution, further obscuring the true prevalence of the condition.
A Call To Action
The evidence linking serotonin to sexual development and the impact of SSRIs on sexual function is clear. Yet, countless individuals have been prescribed these drugs without full disclosure of their potential long-term effects on gender identity and sexual function.
This failure of informed consent is not just an oversight—it's an ethical breach. We should demand immediate action from healthcare providers: full transparency about the known and potential risks of SSRIs, especially during adolescence.
Urgent, well-funded research into Post-SSRI Sexual Dysfunction (PSSD) and the long-term impacts of these drugs on sexual and gender identity development is imperative. Furthermore, a complete overhaul of prescribing practices is necessary, prioritizing patient safety over quick-fix solutions.
The harm inflicted on patients through inadequate information and reckless prescribing must end. We owe it to those already affected and to future generations to confront this issue head-on. The time for willful ignorance is over. We must act now to prevent further harm and to support those already impacted by these life-altering drugs.







Thanks Doc.
There is a huge proportion of Australians on SSRIs which increased a lot in 2020-2021. Physicians were doling them out like candy during lockdowns while we were getting beaten in the street, shot, and arrested for resisting.
I cannot help but think that the widespread 'emotional blunting' due to SSRIs may have contributed to the selfish, zombie-like behaviour of the people who turned their backs to the immense suffering that was occurring. The government was medicating people so that they would not join the resistance.
As an aside, I was speaking to someone who has a child in high school. She said that all the kids want to be on SSRIs to 1. 'fit in with their peers' and 2. get extra accommodations for exams. She said that if a child is on medication for a 'mental illness,' they get a lot more accommodation in school.
Thanks again for the article. Makes me sad that doctors will not read it.
Good article. I’m not sure about causality of SSRI use and transgender identification, though. For sure there is a correlation, but I tend to think they are both results of a common cause, and that the common cause is cultural. My daughter has been transgender identified for five years now. Only after that had been going on for several years did she get on SSRIs. She desperately wanted to be officially diagnosed with something (she tried to convince us she had autism, ADHD, anxiety, depression, and dissociative identity disorder. Eventually she found a psychiatrist who diagnosed her with ADHD, depression, and PTSD). I think this and the transgender identity are both attempts to get validation and understanding for feelings of distress (no distressed teenager wants to be told that their problems aren’t unique or aren’t that bad) and to have a reason to stop trying when things get tough. This is the culture of a significant part of Gen Z - everyone’s on medications, everyone has diagnoses, see how unique and real my pain is, see how you can’t expect anything of me because I can’t do things and it’s not my fault, I have a disability. To add some nuance, some of them really do, but leaning into their problems in this way isn’t helping them learn to use their strengths and work on their weaknesses and be the best they can be. In my opinion it’s these cultural attitudes that have led both to the increase in SSRI use and transgender identification.
Completely agree with you that SSRIs are overused, though! My daughter strongly believes that they help her greatly. I wonder how much of that is a placebo effect.